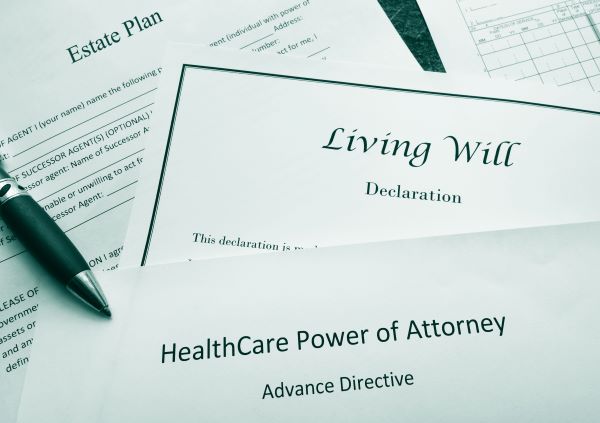
Medical Estate Planning Documents: What You Need to Know
Wills, trusts, and transferring assets are typically thought of when people think of estate planning. However, there is another part of estate planning that doesn’t get as much attention. It concerns advance health care planning. Have you thought about what…